ULTRASOUND GUIDED INJECTIONS FOR MUSCULOSKELETAL CONDITIONS
BY FRED ARNOLD, DC, NMD
Palpation guided injections have been the method to administer regenerative joint injections for decades. Ultrasound guided injections have been gaining in popularity as technology and practitioner’s skills have improved. Each of these injection methods have both advantages and disadvantages.
Today there are a variety of different regenerative joint solutions that are currently being used in practice: prolotherapy, prolozone, platelet rich plasma (PRP), adipose stem cells, bone marrow concentrate stem cells (BMAC), amniotic tissues, alpha-2-macroglobulin and exosomes. These different regenerative joint solutions may be used alone or in combination to improve efficiency.
PALPATION OR LANDMARK GUIDED INJECTIONS
Palpation is an art that involves examination with the hands, of a body to determine its size, shape, firmness or location.1. Musculoskeletal palpation is used to identify the location and abnormalities of different joints to perform palpation guided injections and has been the standard in regenerative joint injections for decades. Regenerative joint practitioners have successfully performed palpation guided regenerative joint injections such as prolotherapy, PRP, prolozone and stem cells. In addition to palpation skills, practitioners also utilize patient history and diagnostic tests such as x-rays and MRI findings. Most of the areas to be injected are painful on palpation and is a help to the practitioner when determining where to inject. Palpation guided injections require a strong understanding of human anatomy.
Advantages of Palpation/Landmark Guided injections include
- Neither patient nor doctor bears the cost burden of an ultrasound machine.
- Palpations guided injections have been successfully performed for decades.
- Easier to learn
Disadvantages of Palpation/Landmark Guided Injections include
- Exact needle placement may not always be performed.
- Patient outcome may be compromised by an inexperienced practitioner.
- Diagnosis of underlying structures is not always accurate
ULTRASOUND GUIDED INJECTIONS
Using the ultrasound for musculoskeletal conditions (MSK) has become increasingly more popular the past few years for both diagnosis and guided injections. Orthopedic Training organizations such as the American Association of Orthopedic Medicine, The Hackett-Hemwell Foundation and the American Osteopathic Association of Prolotherapy Regenerative Medicine Osteopathic now teach ultrasound guided injections as part of their training with regenerative joint injections. Some ultrasound training institutions now offer specific training in MSK and private companies with send experienced technicians to a doctor’s office to assist them with specific injection procedures.
Advantages of Ultrasound Guided injections include
- Exact visual identification of the structure to be injected with immediate assessment of the structures to be injected.

Ultrasound image of the anterior hip joint.
Of all the joints in the body, the hip joint can be the most difficult to treat when there is moderate to advanced degeneration and arthritis. The ultrasound allows for exact placement of the injection needle into the joint capsule.
- Allows for identification of anatomical structures for exact needle placement.

Picture the suprapatellar recess above the knee cap. This is exactly where the needle should be placed for injection of the regenerative joint solution for an intraarticular injection.
- Allows for identification of structures that would not benefit from regenerative joint injections

This picture shows the biceps tendon (arrow) out of the bicipital groove due to a distended and torn transverse humeral ligament.
- Diagnosis can be made of the underlying structures such as the tendons, ligaments, cartilage and bone.
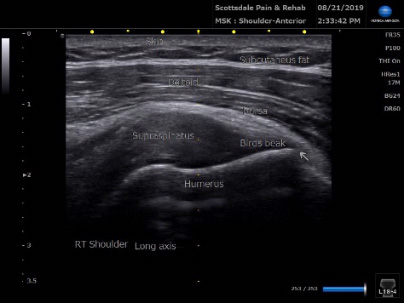
Picture of the supraspinatus tendon of the shoulder and surrounding tissues.
- Comparison views of anatomical structures are readily available.

Right Median Nerve measuring 0.11cm2
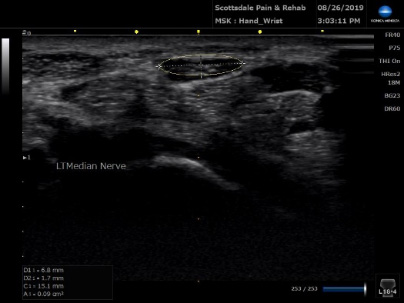
Left Median Nerve measuring 0.09cm2
A median nerve area of less than 0.06cm2 usually excludes carpal tunnel syndrome and an area greater than 0.12 cm2 usually indicates carpal tunnel syndrome. 2
- Overall ultrasound injections are more accurate than palpation or landmark guided injections.
Although, studies are limited, ultrasound guidance-guided injections of both the upper and lower extremities have shown superior benefit to landmark-guided injections. In one study, upper extremity injections included the glenohumeral joint, the subacromial space, the biceps tendon sheath and the joints of the hand and wrist. Lower extremity injections included the knee, ankle and foot.3
- Ultrasound guided injections may be reimbursable by some insurance companies.
- No radiation exposure (compared to x-ray and Computerized Tomography).
- Structures such as tendons are moving in real-time, functionality of structures, range of motion.
Anatomical structures can be evaluated with movement to identify proper functioning. Movement of a body part can identify tears, structural displacements and anatomical anomalies.
- Patients appreciate when the practitioner is able to show them the nature of their problem area and compare progress over time with regenerative joint injection therapies.
Disadvantages of ultrasound Guided Injections include
- There is strong “learning curve” to be able to identify the structures to be injected.
One way to reduce the learning curve is for the practitioner to hire a trained registered musculoskeletal sonographer (RMSKS) on a regular basis. Although, ultrasound training is provided at regenerative medicine conferences, the amount of actual “hands-on” training is limited and often overcrowded to adequately learn this knowledge and skill.
- To the practitioner, there is an additional cost of the ultrasound machine that may range from approximately $30,000 -$50,000.
This can be offset if the office files insurance or charges an additional amount to use the ultrasound machine.
- There may be an additional patient cost to the treatment.
So far, we have not had any patients complain about the additional cost when the ultrasound machine is utilized. They appreciate the improved accuracy and feel their results are improved.
- Limited evaluation of intra-articular structures.
Intra-articular structures cannot be viewed with the ultrasound; however, it is possible to form an opinion of a structure based on extra-articular tissues. Example: a torn meniscus in the knee could present with an extrusion at the joint space and fluid. This is called a “geyser sign”.
- Limited field of view.
The field of view is limited to the placement of the probe; however, the probe can easily be moved to view adjacent structures.
Studies
Ultrasonography in the evaluation and treatment of musculoskeletal conditions is an emerging field in the field of orthopedics. As with any new method in medicine, the number of initial studies comparing landmark guided injections to ultrasound guided injections is limited and vary in the accuracy and benefits of each type of injection.
In a study involving diagnostic injection of the shoulder, the authors state “accuracy is often improved with the use of ultrasonography guidance, although studies differ on the benefits of guided versus unguided injection”.4 In another study, that involved a comprehensive review of the literature, guided injections of the shoulder gleno-humeral joint had higher overall accuracy compared to blind injections. However, the article then states, “nevertheless, in some studies, including a relatively large number of shoulders, blind injections have been proven to be 100% accurate”.5 In a study involving 50 hips that were injected with a contrast, the ultrasound-guided intra-articular hip injection were accurate, efficient and patient friendly. 6
In other studies involving different anatomical structures with both living and cadaveric studies, the results support the accuracy and diagnostic benefits of ultrasound guided injections for the sacroiliac joint 7,shoulder girdle 8, hip 9, and knee.10 Ultrasound guided injections were even more accurate and had greater diagnostic benefits than unguided or fluoroscopy-guided biceps tendon sheath injections.11
As would be expected, the accuracy of ultrasound guided injections is dependent on the user and their experience.12
One common conclusion with most all of the studies is the need for future clinical studies to compare outcomes of palpation/landmark guided and ultrasound guided injections.
Conclusion
Regardless of the research studies, the practitioner should have a firm knowledge of anatomy landmarks as they begin to learn musculoskeletal ultrasound. Palpation skills learned to perform land mark guided injections will be of benefit when ultrasound guided injections are performed.
The practitioner should be able to perform palpation guided injections in addition to ultrasound guided injections. Palpation should always be performed before any type of injection for proper needle placement. Regardless, of which method used, regenerative joint injections provide an alternative to other forms of musculoskeletal treatment such as physical therapy, steroid injections and surgery. The side effects of steroid injections should be reviewed before these injections are performed and surgery should be the last resort for any musculoskeletal procedure.
References:
- Wikipedia, The Free Encyclopedia, Palpation https://en.wikipedia.org/wiki/Palpation, Accessed August 18, 2019
- Jacobson, Jon A., Fundamentals of Musculoskeletal Ultrasound, Philadelphia, PA, Elsevier, 2018: 204
- Daniels EW, Cole D, JacobsB, et al, Existing Evidence on Ultrasound-Guided Injections in Sports Medicine, Orthop J Sports Med, 2018 22;6(2); 2325967117756576
- McFarland E, Bernard J, Dein, et al, Diagnostic Injections About the Shoulder, J Am Acad Orthop Surg, 2017
- Simoni P, Grumolato M, Malaise O, et al, Are blind injections of gleno-humeral joint (GHT) really less accurate imaging-guided injections? A narrative systematic review considering multiple anatomical approaches, Radiol Med, 2017
- Balog TP, Rhodehouse BB, Turner EK, et al, Accuracy of Ultrasound-Guided Intra-articular Hip Injections Performed in the Orthopedic Clinic, Orthopedics, 2017
- De Luigi AJ, Saini V, Mathur R, et al, Assessing the Accuracy of ultrasound-Guided Needle Placement in Sacroiliac joint Injections, Am J Phys Med Rehabil, 2019
- Aly AR, Rajasekaran S, Ashworth N, Ultrasound-guided shoulder girdle injections are more accurate and more effective than landmark-guided injections: a systematic review and meta-analysis, Br J Sports Med, 2015
- Lynch TS, Oshlag Bl, Bottiglieri TS, et al, Ultrasound-Guided Hip Injections, J Am Acad Orhop Surg, 2019
- Lueders DR, Smith J, Sellon JL, Ultrasound-Guided Knee Procedures, Phys Med Rehabil Clin N Am, 2016
- Petscavage-Thomas J, Gustas C, Comparison of Ultrasound-Guided to Fluoroscopy-Guided Biceps Tendon Sheath Therapeutic Injection, J Ultrasound Med, 2016
- To P, McClary KN, Sinclair MK, et al, The Accuracy of common Hand Injections With and Without Ultrasound: An Anatomical Study, Hand (NY), 2017
Richard Kates, RMSKS, provided assistance regarding the identification and accuracy of some of the pictures presented.
With over 28 years of clinical experience, Dr. Fred G. Arnold, D.C., N.M.D specializes in Regenerative Joint Injections. He is Certified in Prolotherapy by the American Association of Orthopedic Medicine (AAOM), A Fellow in Anti-Aging & Regenerative Medicine, A Fellow of American Academy of Ozonotherapy (FAAOM), and Certified in Chelation. He has both a Naturopathic Medical Degree and Chiropractic Degree.